For women, staying in tune with our bodies and managing our unique health needs can be challenging, especially in college. With so much on our plates academically and personally, health can fall to the wayside. However, fostering overall wellness—spiritually, physically, and mentally—is paramount to your ability for success on or off-campus. You can become your own best advocate for yourself and others’ wellness by taking steps to know your body, reach out, share, and discover resources available through your university network and community. Here are three ways to take initiative to be empowered, embrace your needs, and take charge of your wellness in college.
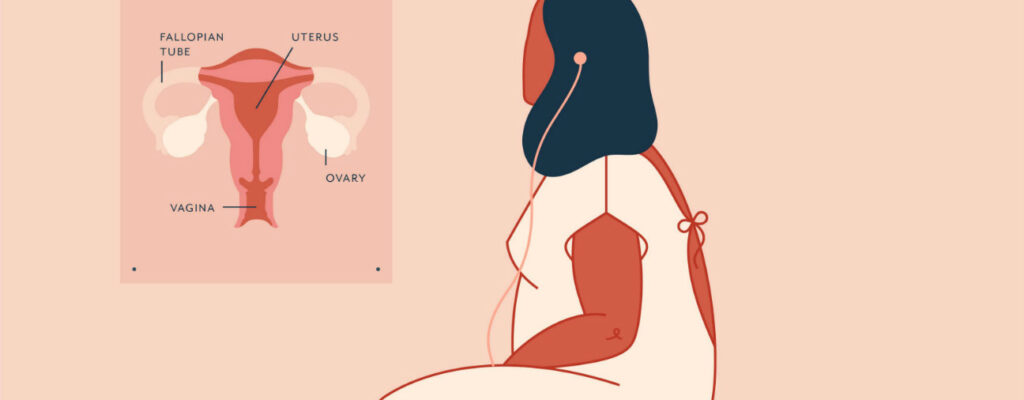
Stay On Top of Your Healthcare Needs
Don’t neglect your wellness check-ins. Becoming wrapped up in the semester may distract you from prioritizing your health and you may forget to keep up with your healthcare visits. Fortunately, there are tools to help keep track of your health needs and make speaking with a healthcare professional more accessible and convenient. Telemedicine in particular can be a great way to consult with a variety of specialists whether you are in your dorm or at home. Speaking with a gynecologist about contraceptives such as an IUD, a dermatologist to help you find a prescription acne medication for pimples, or a therapist to help you with mental health struggles, can all be done via telemedicine. If you happen to feel some anxiety around a health visit, or think that a certain topic may be too taboo to bring up, remember that speaking with a healthcare provider can be empowering and reassuring. A conversation with a healthcare expert can alleviate tension or uncertainty you may be feeling, and talking through your concerns can help you to recognize your stressors and be able to better manage them. Your provider will be understanding and will help you become more confident talking about your health and wellness.
Let’s Talk Stress Management
Stress can be inevitable when the demands of college become a lot to handle. According to a study by The American College Health Association, 48 percent of college women surveyed rated their overall stress levels as more than average. Such stress can have a significant impact on your overall health and academics. The uncertainty introduced by the COVID-19 pandemic has exacerbated the process. College can be an overwhelming place for women who juggle multiple responsibilities. From cramming for your next exam to getting involved in community work, athletics, or passion projects, it can often seem like there is so much to tackle at once. However, remind yourself that you are indeed accomplished and that you should not measure success by how much you are doing. Be proud, own your success, and empower yourself by being in control of striking a balance. Pause for a moment, take a breath and remember that stress management is key to your health and happiness. Prioritize working in stress management strategies into your day. Some great strategies to try out include:
- Bullet journaling
- Deep breathing
- Enjoying a podcast
- Listening to music
- Reading
- Trying a self-care box
- Watching your favorite YouTube channel
Truthfully, this list could be endless, so what really matters is finding a technique that engages and resonates with you.
Uplift Yourself and Other Women
The impacts of social isolation on mental health are widespread nowadays due to the pandemic. It can be mentally draining to spend most of your time in class just to return to your space at the end of the day. Therefore, it is vital to maintain connections and interact safely with your peers. What better way is there to connect with others than through women empowering other women? Check out your campus groups to see if there are any related to women’s rights or social justice. You can also try to find women’s groups in your field of study. These organizations may meet virtually on a regular basis, or maybe still are able to meet in small groups in person. It can be a great way to champion women’s causes, network, and form meaningful connections with others. On a personal level, getting involved can help you to feel more confident and lift your spirits. We all know how good it feels when another woman compliments us, or how satisfying it is to work together towards a cause. Let’s mentor and cheer each other on.
Empowering yourself to take care of your wellness in college is rewarding. Learning more about your body, wellness strategies, and how to bring positivity into your life can transform your entire college experience. Be an advocate for yourself but also try to empower others as well. Don’t hesitate to share what you know, initiate a conversation, start a new group, and spread awareness on great women’s causes. When it comes to advocating for yourself and other women in your community, college is a great place to start.
Featured Image by showfantasy