Analyses of immune dysfunction in severe COVID-19 patients have revealed dysregulated immune responses including abnormal myeloid cell subsets (Schulte-Schrepping et al., 2020; Silvin et al., 2020), HLA class II downregulation on monocytes (Wilk et al., 2020), lymphopenia (Cao, 2020), and elevated levels of inflammatory cytokines (Del Valle et al., 2020). However, presentation of COVID-19 is heterogeneous and as such, understanding the immune response across varying disease severities is important to predict disease prognosis and provide effective treatment given the stage of disease.
A recent study published in Cell aims to understand the relation between elevated inflammation signals, plasma metabolite composition, and immune cell dysfunction by analyzing plasma and PBMCs (peripheral blood mononuclear cells) from patients across all levels of disease severity (Su et al., 2020). The researchers collected plasma and PBMCs from 258 healthy adult donors and 139 COVID-19 adult patients representative of distinct disease stages. Blood was drawn from each COVID-19 patient at two timepoints, once at initial clinical diagnosis and again a few days later. Disease severity score was based on the WHO ordinal scale (WOS) and was recorded at the time of each blood draw.
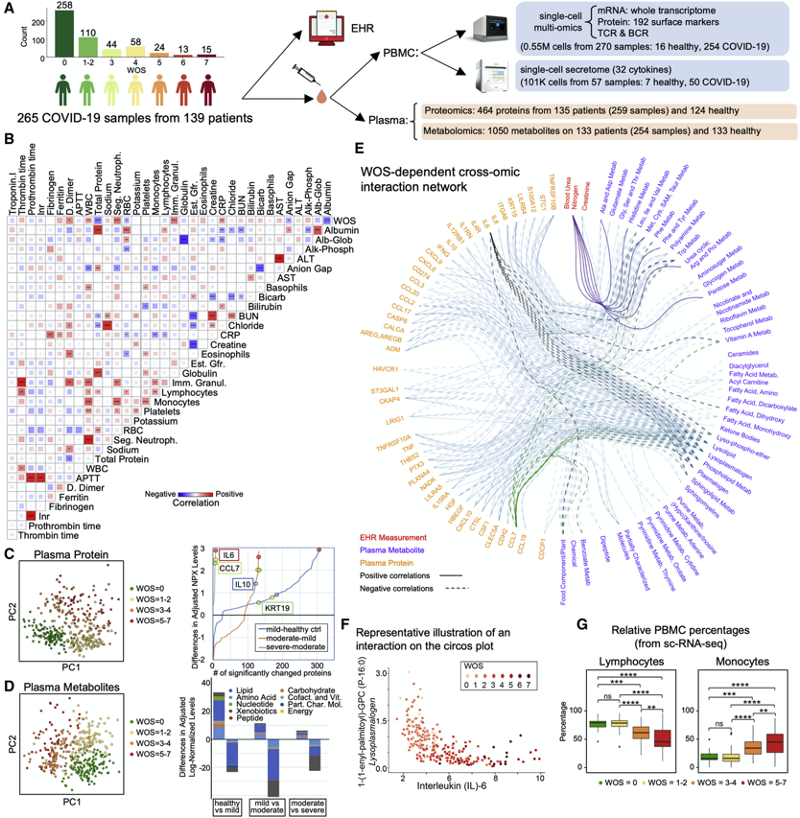
Analysis of percentages of various cell types relative to disease severity through sc-RNA-seq indicated that the most significant change in levels of lymphocytes and monocytes occurs between mild and moderate disease across individuals (Figure 1G). The scientists found that compared to individuals with mild disease, those with moderate disease had lower relative percentages of CD4+ T cells, NK cells and CD8+ T cells. B cell percentages did not significantly vary across disease severity, a finding consistent with previous reports (Zhang et al., 2020). The change in plasma proteins and metabolites were also analyzed between patient samples of varying levels of disease severity (Figure 1C and 1D). 500 proteins and 1,000 metabolites were analyzed from patient plasma samples. The metabolite composition was evaluated by metabolic-change scores and interestingly found distinct downregulation of fatty acids and a loss of circulating metabolites in patients with moderate disease relative to mild. The authors indicate that the elevated cytokine levels in those with moderate disease, including CCL7 and IL-6, and decreased metabolic resources could be indicative of a pro-inflammatory state that could distinguish mild cases of COVID from moderate cases.
The paper goes on to further detail novel immune subsets that emerge in moderate cases and reveals correlations in response between moderate and severe disease. Overall, through characterization of different immune signatures, the authors highlight a distinct immunological shift between mild and moderate infection. The results of this study could provide valuable information for clinicians in differentiating people with mild and moderate COVID-19 and direct medical treatment of patients.
References
Su et al., Multi-Omics Resolves a Sharp Disease-State Shift between Mild and Moderate COVID-19, Cell (2020), https://doi.org/10.1016/j.cell.2020.10.037
Schulte-Schrepping, J., Reusch, N., Paclik, D., Baßler, K., Schlickeiser, S., Zhang, B., Kra ̈mer, B., Krammer, T., Brumhard, S., Bonaguro, L., et al. (2020). Severe COVID-19 Is Marked by a Dysregulated Myeloid Cell Compartment. Cell 182, 1419–1440.
Silvin, A., Chapuis, N., Dunsmore, G., Goubet, A.-G., Dubuisson, A., Derosa, L., Almire, C., He ́ non, C., Kosmider, O., Droin, N., et al. (2020). Elevated Cal- protectin and Abnormal Myeloid Cell Subsets Discriminate Severe from Mild COVID-19. Cell 182, 1401–1418.
Wilk, A.J., Rustagi, A., Zhao, N.Q., Roque, J., Mart ́ınez-Colo ́ n, G.J., McKech- nie, J.L., Ivison, G.T., Ranganath, T., Vergara, R., Hollis, T., et al. (2020). A sin- gle-cell atlas of the peripheral immune response in patients with severe COVID-19. Nat. Med. 26, 1070–1076.
Zhang, J.-Y., Wang, X.-M., Xing, X., Xu, Z., Zhang, C., Song, J.-W., Fan, X., Xia, P., Fu, J.-L., Wang, S.-Y., et al. (2020). Single-cell landscape of immunological responses in patients with COVID-19. Nat. Immunol. 21, 1107–1118.
Leave a Reply