Endometriosis affects approximately 1 in 10 women, disproportionately affecting women in their 30s and 40s. For most individuals, getting diagnosed with endometriosis is a difficult process. On average, it takes anywhere from 3 to 11 years after the onset of symptoms to reach the final diagnosis. Social media is rife with personal accounts of healthcare failures exacerbating endometriosis. For example, YouTubers who have gone through the diagnostic journey themselves shed light on why it takes such a long time to reach a diagnosis, whether it be doctors dismissing their pain or reaching another diagnosis that might explain the symptoms that they are experiencing. Buzzfeed’s As/Is channel on YouTube uploaded a video in 2019 titled “A Week In My Life With Endometriosis,” which documented one individual’s daily life while they deal with this condition. Clips of her laying in bed with loose, stretchy pants, shopping for “safe foods,” and keeping a heating pad on while sitting at her work desk felt extra relatable to me, as there are days where my pain confines me to oversized sweatshirts and loose leggings but I still have to attend classes or take care of errands. “The extra steps that I have to take every single day just to be comfortable, just to exist in a way that’s comfortable to me, is something that I wish the average person understood a little bit better” is a sentence that still resonates with me to this day.
Like the woman in the YouTube video, my mother ranks among the countless people who have suffered from both the physical and institutional consequences of endometriosis. Since the age of 18, she suffered from bad periods. “My cramps were so severe that I would double-over in pain and take an unrecommended amount of aspirin just to get by,” my mom explained to me. This pain stayed for another 3 years, until she started using birth control pills to prevent an unplanned pregnancy. Four to five years later when my parents started to discuss having kids and my mom stopped the birth control, the bad periods returned and her pain was at an all-time high. When she talked to her gynecologist at the time about her symptoms, she was told that she was just experiencing severe hormone imbalance due to stopping birth control. “Every woman has cramps,” they said to her. It took switching to a new gynecologist and eventually being referred to a fertility specialist at age 27 for my mom to be diagnosed with severe endometriosis.
My story is a little bit different from my mom’s. I started experiencing bad periods when I was around 12 years old, and at age 14, I went to my mom’s OB/GYN so that I could be given the Nexplanon birth control implant. From the next 4 to 5 years, my birth control seemed to work wonders for me. However, in the past two years I’ve noticed that some of my previous symptoms are returning, I’m experiencing new symptoms I haven’t before, and something doesn’t feel right. I am 21 years old, and I am experiencing a lot of the same symptoms my mother was experiencing right before her diagnosis. In addition to talking to my mom, I’ve started to do my own research, and here is what I have found so far.
So… what exactly is endometriosis?
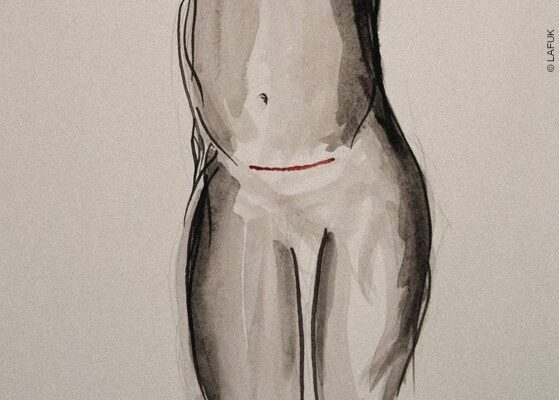
Endometriosis is a condition in which endometrial-like tissue that typically lines your uterus starts to grow outside of the uterus. Endometrial tissue in your uterus thickens each month and will break down and shed with your menstrual cycle. However, the endometrial-like tissue that grows outside of the uterus on your pelvic organs (or even outside the pelvis region entirely) has no way to shed your body, so it becomes trapped and eventually becomes irritated, leading to scar tissue and adhesions. It is the scar tissue and adhesions that often are the source of the pain people with endometriosis commonly experience, and also the source of fertility problems that may only be discovered when one is planning to have children.
What does endometriosis feel or look like?
While endometriosis can vary from person to person, there are many common symptoms that individuals can face. These symptoms include:
- Painful periods
- Pain with sexual intercourse
- Pain with bowel movements or urination
- Excessive bleeding during or between periods
- Infertility
- Fatigue, diarrhea, constipation, bloating, nausea, headaches/migraines, and more
It should also be noted that the stage of endometriosis one may get diagnosed with may not correspond to an individual’s pain levels or experience of other symptoms.
How is endometriosis diagnosed, and why does it usually take so long?
To diagnose endometriosis and rule out any other conditions, your doctor will typically ask you to describe all of the symptoms that you are experiencing and will conduct a variety of tests, such as pelvic exams, abdominal and/or vaginal ultrasounds, and MRIs. With all of that said, laparoscopies are often referred to as the “gold-standard” for official diagnosis, as this procedure allows doctors to see the inside of your abdomen and see if there is any endometrial tissue growing outside of the uterus, which is often removed at the same time. Biopsies are sometimes performed during these laparoscopies so that the tissue can be tested later in the lab and the diagnosis can be histologically confirmed. Laparoscopies also allow for doctors to determine the stage of endometriosis, ranging from stage 1 (minimal) to stage 4 (severe).
Diagnosis often takes such a long time because endometriosis and its symptoms can be confused with a number of other conditions and diseases, including pelvic inflammatory disease, ovarian cysts, and irritable bowel syndrome. Pain can sometimes be dismissed by doctors that think it is “normal,” or the condition may not even be an issue until an individual starts to encounter fertility issues.
How is endometriosis treated? Is there a cure?
Unfortunately, there is no cure for endometriosis. However, there are many effective treatments that are available today, and because endometriosis is unique to each individual, individualized treatment plans are important. Treatment for endometriosis typically involves (but is not limited to) laparoscopic surgeries, pain medication, and/or hormone therapy. Some individuals may continue to experience pain or have pain return years after treatment, which can be the case when endometrial tissue that was not visible and/or removable during initial surgery, in which medication or even a hysterectomy is the next step to manage symptoms.
For my mom, most of her symptoms alleviated three different times – when she became pregnant, after she started DepoProvera birth control, and when she entered menopause. Countless people have anecdotes of their endometriosis symptoms improving after becoming pregnant, but the problem with this is that many are infertile as a result of this condition and have a difficult time conceiving, and there are also many who do not plan on having any children for a while or ever. As for my own journey and my future, I do not plan on ever having children and I think that sometimes my symptoms or treatment options have been overlooked multiple times due to the fact that I am not actively working to become pregnant. Additionally, I am not interested in starting DepoProvera since I am happy with my current form of birth control, and as a 21-year-old, I am not even close to starting menopause. However, after actively advocating for myself at my appointments with my gynecologist, I am in the process of being referred to a surgeon who can do the diagnostic laparoscopic procedure for me at the end of this year. Both my mom and I have our concerns about having the surgery done, but we know that it is important for me to get answers for the sake of my own health and work towards a future with minimal pain. In the past year or so, I’ve learned that not every person’s case of endometriosis is the same, and with that knowledge in mind, I want to be able to share important information and spread awareness so that people like me will know when to start a conversation with their doctor.
For more information, you can visit acog.org or find an OB-GYN here.